Everyone experiences ups and downs in their mood, are sometimes overly anxious and worried, or have trouble with sleep. Most of these experiences do not suggest a psychiatric disorder but are rather part of the human condition. However, when negative or extreme mood or anxiety states persist and cause disability and/or distress, the underlying cause or causes require attention and treatment. One relatively common cause of these types of symptoms is bipolar disorder.
- Bipolar disorder affects up to perhaps 3% of the population, so it is relatively common compared with other major psychiatric conditions; for example, schizophrenia occurs in about 1% of people.
- Historically, bipolar disorder was referred to as manic-depressive illness, with the modern nomenclature arising in 1957, to separate mood disorders in people who only experienced depression from those who also experienced mania. The name is a little misleading as it is possible for symptoms of mania and depression to co-exist, that is, they do not always exist separately and commonly overlap.
- The predominate symptoms tend to define the mood state as depressed or manic, although at times this distinction is not possible and is referred to as a mixed state. Regardless, the occurrence of mania or hypomania (or a mixed state when mania criteria are met) defines the existence of bipolar disorder.
- Hypomania and mania share the same symptoms, with the difference between them being one of severity of impairment; specifically, mania is functionally impairing whereas hypomania is not.
Bipolar disorder includes several subtypes; the most common of these are bipolar disorder, type I (bipolar I disorder), bipolar disorder type II (bipolar II disorder) and cyclothymia. In young people, bipolar II disorder and cyclothymia may be transitional states toward bipolar I disorder, but once people are adults (e.g., mid-20’s), these conditions tend to remain relatively constant over the lifespan. All of these disorders, once they emerge, tend to be lifelong conditions requiring ongoing management. The good news is that management of these illnesses is possible to permit people with the disorders to live meaningful and fulfilling lives.
Bipolar I disorder is defined by the occurrence of mania. Mania is an activated mood state characterized by excessive reward seeking accompanied by increased behavioral activation and euphoric, elevated, irritable, or labile mood.
Signs and symptoms of a manic episode can include the following:
- Excessive pursuit of rewards or perceived rewards despite negative consequences, such as spending sprees, initiating poorly planned projects, excessive risk taking and hypersexuality.
- Excessively high, euphoric, or elevated mood or, concurrently or alternatively, extreme irritability or mood lability.
- Increased energy, activity, and restlessness.
- Racing thoughts and talking very fast, jumping from one idea to another
- Distractibility, inability to concentrate.
- Decreased need for sleep (not simply poor sleep, but the belief that sleep is not necessary).
- Unrealistic beliefs in one's abilities or importance.
- Poor judgment and insight; people are sometimes unaware of their symptoms.
- Abuse of drugs of all types, although usually, what is most readily available.
- Provocative, intrusive, or aggressive behavior.
- Psychotic symptoms commonly occur in mania and include delusions (fixed, false beliefs, such as persecution by the CIA), hallucinations, or disordered thinking.
Bipolar II disorder is defined by the occurrence of hypomania plus at least one episode of depression (please refer to the Depression section on this website for details). As noted, the symptoms of hypomania are exactly those for mania, but are less severe so do not cause significant functional impairment and psychosis is not present; however, they must be sufficiently present to represent a change from the person’s typical behavior. This distinction between mania and hypomania can be difficult (as impairment is somewhat subjective), and people with bipolar I illness may experience episodes of hypomania as well as mania, confusing diagnoses at times.
Cyclothymia is a condition with at least two years of hypomanic and depressive symptoms that never progress into either a major depressive or hypomanic or manic episode (i.e. bipolar I and II disorder). The mood cycling needs to cause distress or some level of functional impairment. As with bipolar II disorder, making this diagnosis can be challenging, as people with cyclothymia typically do not seek treatment. Together, these diagnoses can be subtle and difficult to make, so are best done with a psychiatrist with some expertise in managing bipolar disorder.
As noted, although bipolar disorder(s) can be effectively managed, they can also be sources of significant suffering and mortality. The suicide rate in bipolar disorder is among the highest of any medical and psychiatric condition, perhaps as high as 10-15% of affected individuals. Bipolar disorder is also recognized as one of the top 10 most disabling conditions in developed countries worldwide. Much of the disability arises from the frequent depressive episodes, which often dominate the long-term course of illness, but co-occurring illnesses are also common. Anxiety disorders especially common, as is attention deficit hyperactivity disorder (ADHD); when these co-occur with bipolar disorder, additional treatment is often needed including medications and evidence-based therapies. Additionally, a diagnosis of bipolar disorder increases the risk of drug and alcohol abuse, smoking, obesity, cancer, and cardiac disease, all of which increase the risk of premature death and disability. Through evidence-based thoughtful treatment and integration with good primary care, much of this risk can be effectively managed.
Bipolar disorder is strongly familial, with most of the risk being genetic (about 85%). It is a neurodevelopmental condition that emerges typically in adolescence or young adulthood. The initial course of illness may exhibit progressive decreases in well periods, called “euthymia”, leading ultimately to annual recurrences of mania and/or depression. Effective treatment can decrease the likelihood of new episodes, but we do not yet know how to prevent illness progression, or how to prevent it in the first place. Early detection and treatment do improve long-term outcome, so in families with bipolar disorder, keeping an eye on youth is advised with a low threshold to seek psychiatric help if problems arise. It is better to be told there is nothing to worry about than to miss an opportunity for early intervention.
Treatment
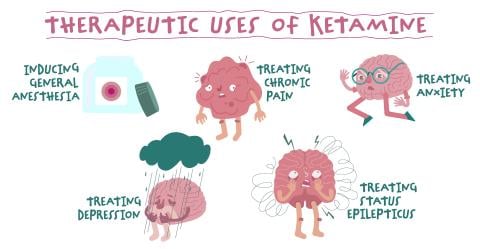
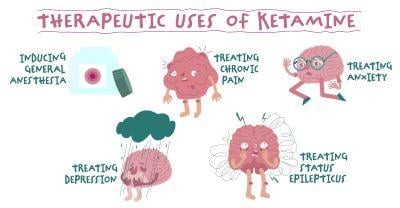
The treatment of bipolar disorder requires both medications and therapy for best outcomes. Most people can be managed with three or fewer medications, so whenever a fourth is being considered, re-evaluation is recommended. The backbone of medication treatment consists of various mood stabilizing/anti-manic drugs including lithium, divalproex sodium, several second-generation antipsychotics and several anti-epileptics.
Medication choices are typically driven by response and tolerability within an individual, requiring some evidence-based and informed trial and error. Antidepressants are much less useful than they were once thought to be, but may have a role in individuals with anxiety disorders or treatment resistant depression (to the mood stabilizers).
Several evidence-based psychotherapies, such as cognitive behavior therapy (CBT) or family-focused therapy, are also helpful. The diagnosis and treatment of bipolar disorder is complex, requiring psychiatric and other mental health professionals experienced in its management. With good treatment, as noted previously, people with bipolar disorder can typically live the lives that they hoped prior to getting ill. Outcomes can be good.
ADAA Resources:
- Living Well with Bipolar Disorder - personal story by Gabe Howard
- What We Get Wrong About Being Bipolar | Opinion - Newsweek, March 29, 2024 - Gabe Howard
- As an Athlete, I Needed to Win the Mental Health Game, personal story by Alexis Belton
- Find Your Therapist Directory
- What is Bipolar Disorder?, video
- Bipolar Disorder Explained, video
- My Child Has Mood Swings: How Do I Know if It’s Bipolar Disorder, and What Do I Do? Diagnosis and Treatments for Bipolar Children & Adolescents
Resources by the ADAA professional community:
- Misconceptions About Bipolar I Disorder, HealthCentral, Simon Rego, PsyD, ABPP